Latest Blogs
Blogs that we created only just for you. Get ideas and information that might help you to decide what types of services that your body needs.
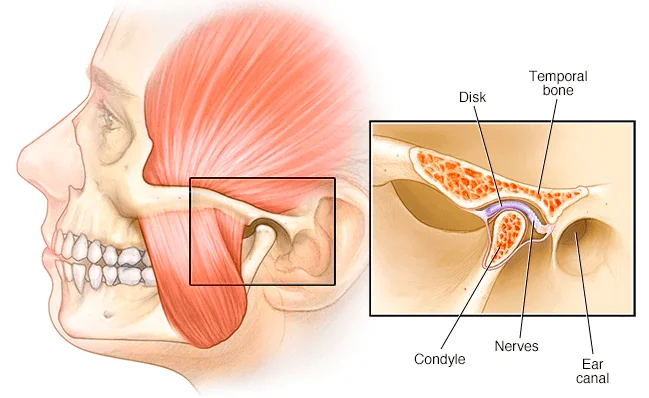
The Temporomandibular Joint is a hinge that connects the jaw to the temporal bones of the skull, which...
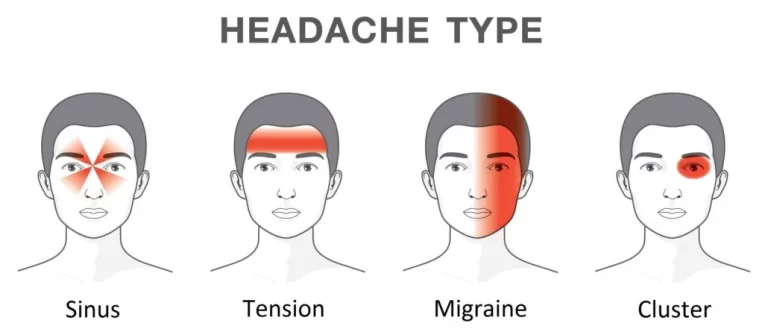
Headaches & Migraine
Headaches are one of the most frequent complaints. Narrowly defined, a Headache...

Are you experiencing aches and pains and seeking an alternative treatment to medication or surgery?...

PART 1 – INTRODUCTION
For the elderly population or those with a sports injury or chronic musculoskeletal...

Carpal tunnel syndrome (CTS) is a condition that affects your hand and wrist, causing pain, numbness,...

Scoliosis is a spinal condition that affects the curvature of the spine. Those with this condition...

At Orchard Health Clinic, our osteopaths are trained to diagnose and treat various medical conditions...








