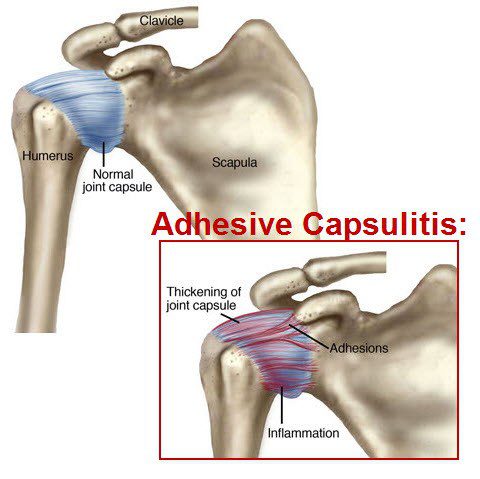
Frozen shoulder, also known as adhesive capsulitis, is a condition where the shoulder joint becomes stiff and painful due to inflammation and capsular contracture. Over time, the joint capsule thickens and tightens, limiting movement and causing significant discomfort.
Neglecting a frozen shoulder can lead to long-term mobility issues and chronic pain, which may impact daily activities and overall quality of life. Identifying and addressing the condition early can prevent complications and help restore full function to the shoulder.
If you’re looking for frozen shoulder treatments in Singapore, seeking care from experienced specialists can make all the difference. At OHC, our team of frozen shoulder experts is dedicated to providing tailored care for your recovery.
What are the Symptoms of Frozen Shoulder?
The symptoms of a frozen shoulder can develop gradually and worsen over time, significantly affecting your daily life. Key signs to watch for include:
- Dull, aching shoulder pain: A persistent discomfort that worsens with movement, particularly when lifting the arm overhead.
- Limited shoulder movement: A noticeable reduction in your ability to move the shoulder freely, especially for overhead or rotational movements.
- Difficulty with everyday tasks: Simple activities like brushing your hair, putting on shirts, or fastening a bra may become difficult due to stiffness.
- Pain while sleeping: The pain may intensify when lying on the affected shoulder, leading to disrupted sleep.
As a frozen shoulder progresses, stiffness and reduced mobility can make even basic actions feel challenging. Early intervention and targeted frozen shoulder treatments are essential for alleviating pain and restoring function. If you’re experiencing any of these symptoms, it’s important to seek professional care from an osteopath in Singapore. Contact us today for personalised treatment options.
Diagnosing Frozen Shoulder
Here’s a comprehensive guide to understanding how healthcare professionals diagnose frozen shoulder:
1. Clinical Assessment: During the evaluation, the healthcare professional will review your medical history, inquire about symptoms, and conduct a thorough physical examination of your shoulder joint.
2. Range of Motion Testing: This involves assessing your ability to move the affected shoulder in various directions, noting any limitations, stiffness, or pain during movement. Restricted range of motion, particularly in outward rotation and abduction, is a hallmark feature of frozen shoulder.
3. Pain Assessment: Patients with frozen shoulder typically report pain that worsens with movement and may radiate down the arm. The healthcare provider will inquire about the onset, duration of your discomfort, and factors associated with the pain.
4. Diagnostic Imaging: While not always necessary, diagnostic imaging studies such as X-rays, ultrasound, or magnetic resonance imaging (MRI) may be ordered to further evaluate your shoulder joint and rule out other potential causes of symptoms before commencing frozen shoulder treatment.
Understanding the Risk Factors of Frozen Shoulder
Several risk factors can predispose individuals to developing shoulder issues like frozen shoulder. Recognising these factors is essential for early intervention and shoulder pain relief.
1. Prolonged Immobility:
Extended periods of shoulder immobility, whether from post-surgical recovery, arm fractures, or prolonged inactivity, can significantly increase the risk of developing a frozen shoulder. When the shoulder is left inactive, the shoulder capsule tightens and constricts, leading to stiffness and a limited range of motion. Movement is key to maintaining joint mobility, and even light exercises can help prevent the onset of a frozen shoulder by keeping the shoulder joint active.
2. Underlying Medical Conditions:
Certain medical conditions such as diabetes, thyroid disorders, cardiovascular disease, and autoimmune conditions can elevate the risk of a frozen shoulder. These conditions may disrupt normal joint function, contributing to inflammation and thickening of the shoulder capsule. Managing these conditions effectively through therapy for discomfort or specific chronic shoulder pain solutions can play an essential role in reducing the risk of developing a frozen shoulder.
3. Age and Gender Factors:
Frozen shoulder is more common in individuals aged 40 and above, particularly in women, especially those experiencing hormonal changes related to menopause. Hormonal fluctuations and age-related changes in connective tissue metabolism can contribute to stiffness and reduced joint mobility. Early intervention, including targeted exercises and therapies, can help improve flexibility and reduce the risk of complications.
4. Trauma or Injury:
Trauma such as falls or shoulder injuries can increase the risk of a frozen shoulder. The resulting inflammation and tissue damage can lead to the formation of scar tissue within the shoulder joint, restricting movement and causing pain. After an injury, seeking chronic shoulder pain solutions or therapy for shoulder pain relief is crucial in managing recovery and restoring function to the shoulder joint.
Understanding these risk factors can help you identify if you’re at a higher risk of developing a frozen shoulder. Early diagnosis and intervention, such as seeking shoulder pain relief treatments in Singapore, can prevent further complications and restore range of motion. For more information on effective treatments, explore our services.
Causes of Frozen Shoulder
A frozen shoulder arises when the connective tissue capsule surrounding the shoulder joint thickens and tightens, limiting joint mobility. While the exact cause remains uncertain, prolonged shoulder immobility, such as after surgery or an arm fracture, is a common trigger. Factors like genetic predispositions or underlying medical conditions may also play a role. Traumatic incidents can also further exacerbate the condition, leading to stiffness and reducing range of motion.
Identifying the Three Stages of Frozen Shoulder
A frozen shoulder progresses through three distinct stages, each with its own symptoms and challenges. Understanding these stages can guide your treatment approach and provide clarity on what to expect throughout your recovery process.
Stage 1 Freezing:
During the “freezing” stage, shoulder pain gradually intensifies, and the range of motion begins to decrease. As the pain worsens, stiffness sets in, making it harder to move the shoulder freely. This stage typically lasts between 6 weeks to 9 months and may require exercises and therapy to help manage pain.
Stage 2 Frozen:
The pain may subside somewhat in the “frozen” stage, but the stiffness remains, significantly limiting joint mobility. Simple tasks can become challenging, and daily activities such as dressing or lifting objects may be hindered. This stage can last from 4 to 6 months, and chronic shoulder pain solutions may be necessary for relief during this period.
Stage 3 Thawing:
The “thawing” stage marks a gradual improvement in shoulder motion and strength. Range of motion slowly returns, and over time, the shoulder begins to regain its normal function. Complete recovery may take anywhere from 6 months to 2 years, depending on the severity of the condition.
Proper treatment and shoulder pain relief therapy during each stage are essential for long-term recovery and preventing further stiffness. Early intervention can help you regain shoulder function and ease discomfort more effectively.
If you are experiencing any of these symptoms, consult a healthcare professional for an accurate diagnosis and personalised frozen shoulder treatment plan in Singapore tailored to your needs.
Can My Frozen Shoulder Be Treated?
Yes, a frozen shoulder can be treated effectively through a range of therapies aimed at reducing pain, improving joint mobility, and restoring the range of motion. Physical therapy plays a central role in managing this condition, and treatment varies depending on the stage of the frozen shoulder.
Treatment in Stages 1 & 2: Focus on Pain Relief and Mobility
During the early stages of a frozen shoulder, the main focus is on managing shoulder pain relief and maintaining as much mobility as possible. Exercises, manual therapy techniques, and modalities like heat and ice treatments are used to relax muscles and alleviate discomfort. These treatments help prevent further loss of motion and manage the increasing stiffness in the joint. A gentle home exercise programme will also be introduced, encouraging safe healing while maintaining flexibility.
Treatment in Stage 3: Restoring Motion and Strength
In the later stages, the primary goal shifts to restoring joint mobility and increasing flexibility. Manual therapy becomes more intense, and stretching exercises are introduced to encourage greater shoulder movement. Strengthening exercises targeting the shoulder and core muscles help rebuild strength and stability, supporting an improved range of motion. As healing progresses, functional training becomes a key part of the treatment, ensuring that normal shoulder mechanics are restored.
Physiotherapy for Comprehensive Treatment
Physiotherapy is a vital component of frozen shoulder treatment, offering targeted techniques to alleviate chronic shoulder pain and improve range of motion. Through a combination of manual therapy, exercises, and therapy for discomfort, physiotherapists design personalised plans that address the specific needs of each patient. If you’d like to learn more about how physiotherapy can help with a frozen shoulder, check out our Comprehensive Guide to Physiotherapy.
What Else Can I Do to Alleviate Frozen Shoulder Pain?
In addition to seeking professional treatment, there are several strategies you can incorporate into your daily routine to help alleviate frozen shoulder pain and improve joint mobility. These complementary approaches can support your recovery, reduce stiffness, and enhance your range of motion.
1. Regular Exercises
Gentle exercises designed to stretch and strengthen the shoulder are essential for managing a frozen shoulder. Regular movement helps prevent further stiffness, promotes shoulder pain relief, and gradually restores flexibility. A combination of stretching and strengthening exercises can improve joint mobility over time.
For a guide to effective exercises, check out our article on 4 Exercises to Relieve Frozen or Stiff Shoulders.
2. Heat and Cold Therapy
Alternating between heat and ice can provide relief from pain and inflammation. Heat treatments help to relax tight muscles and prepare the shoulder for movement, while cold treatments reduce swelling and numb the area to alleviate discomfort. This combination can be highly effective in managing shoulder pain and improving range of motion.
3. Gentle Stretching
Incorporating gentle stretching into your daily routine helps reduce stiffness and increase flexibility. Focus on stretches that target the shoulder area, ensuring you don’t overexert the joint, which can cause further damage. Regular stretching, under professional guidance, can speed up the healing process and maintain the shoulder’s range of motion.
4. Ergonomic Adjustments
Pay attention to your posture and how you use your shoulder throughout the day. Minor ergonomic adjustments at work or home can reduce strain and discomfort, supporting long-term healing. Proper posture and using assistive devices can prevent unnecessary stress on the shoulder joint, contributing to shoulder pain relief.
These strategies, combined with professional care, can significantly improve your recovery from a frozen shoulder.