What is TMJ Disorder?
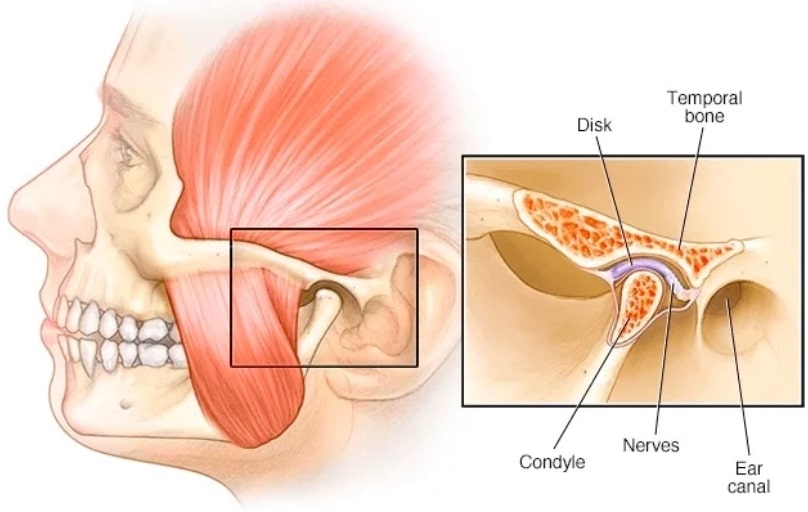
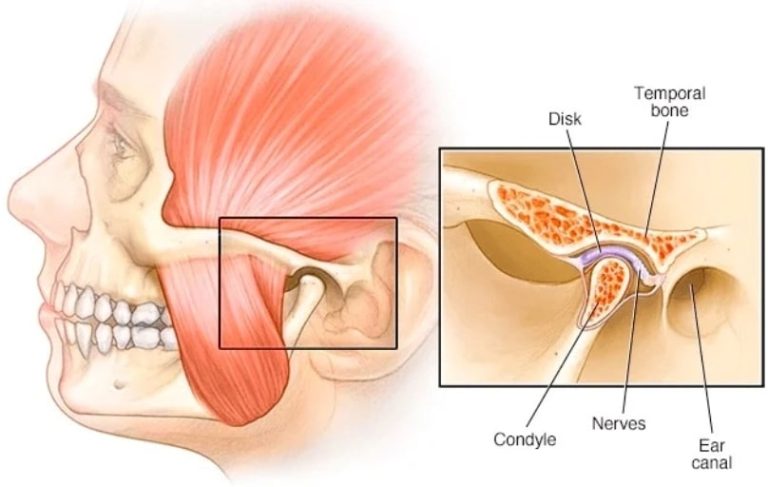
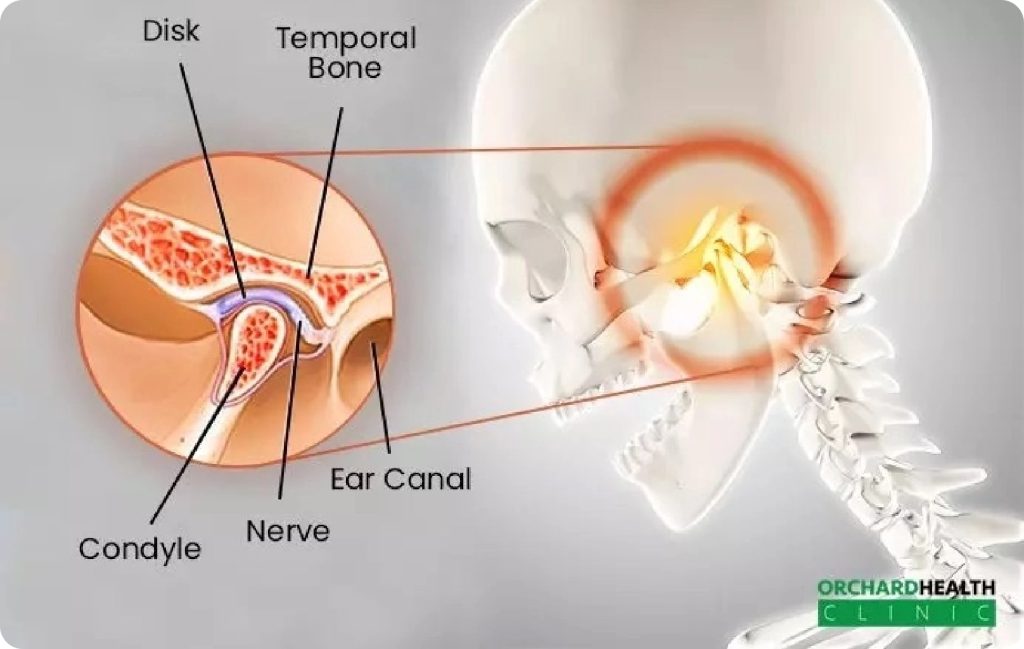
If you’re experiencing persistent pain or discomfort in your jaw, it may be a sign of Temporomandibular Joint (TMJ) Disorder. But what is TMJ disorder, and how does it affect you? This condition impacts the hinge joint connecting your jaw to the temporal bones of your skull, often causing pain during activities like chewing, speaking, and yawning. Left untreated, TMJ disorder can significantly disrupt daily life, but the good news is that effective, non-invasive treatments are available at Orchard Health Clinic.
At Orchard Health Clinic, we specialise in targeted TMJ disorder treatments designed to relieve pain, restore natural jaw function, and help you regain your quality of life. Our expert team takes a multidisciplinary approach, integrating physiotherapy, manual therapy, and advanced techniques such as shockwave therapy to treat the root causes of TMJ disorder—providing long-lasting relief and effective recovery.
Why Choose Orchard Health Clinic for TMJ Treatment?
1. Comprehensive, Individualized Care
We understand that every TMJ disorder is different. Our team provides personalized treatment plans tailored to your specific needs. We carefully assess your symptoms, the underlying causes of your condition, and your lifestyle to ensure our treatment addresses the core of the problem.
2. Multidisciplinary Approach for Optimal Recovery
Orchard Health Clinic integrates multiple therapeutic techniques to provide a holistic treatment for TMJ disorder:
- Physiotherapy to improve jaw flexibility and reduce pain
- Manual Therapy to restore normal joint movement and break down scar tissue
- Shockwave Therapy to promote healing through enhanced blood flow and pain relief
3. Cutting-Edge Technology and Techniques
We offer advanced treatments such as shockwave therapy, which is proven to stimulate healing, reduce inflammation, and improve TMJ mobility. This non-invasive, highly effective approach accelerates recovery and minimizes the need for surgical intervention.
4. Experienced Specialists
Our highly trained physiotherapists and healthcare professionals have extensive experience in managing TMJ dysfunction. We focus on providing effective, non-invasive solutions that address the root causes of your discomfort.
TMJ Disorder Causes
Temporomandibular Joint (TMJ) Disorder can arise from various factors affecting the jaw joint and surrounding muscles. It may lead to discomfort, restricted movement, and clicking or popping sounds in the jaw. Some TMJ Disorder causes are:
Teeth Grinding (Bruxism)
- Teeth grinding creates continuous pressure on the jaw muscles and joints, which can contribute to the causes of the TMJ disorder.
- The friction from grinding can cause gradual wear of the cartilage within the joint.
Malocclusion (Misalignment of Teeth)
- The misalignment of teeth results in uneven chewing forces.
- This imbalance can place extra stress on the TMJ, which leads to muscle tension and jaw discomfort.
Jaw Injury or Trauma
- Injuries such as fractures or dislocations can directly harm the TMJ.
- This damage causes a disruption in the alignment and function of the joint, leading to TMJ disorders and related issues.
Arthritis
- Arthritis leads to the degeneration of cartilage and bone in the TMJ.
- As the cartilage breaks down, the bones may begin to rub against each other, causing inflammation and pain, which causes the TMJ disorder.
Stress
- Stress can increase tension in the jaw and surrounding muscles.
- This added strain can contribute to discomfort and dysfunction in the TMJ.
Genetic Predisposition
- Inherited traits, such as variations in jaw structure or tooth alignment, may cause some individuals to be more prone to TMJ disorder.
- These genetic factors can increase the likelihood of developing TMJ-related issues.
TMJ Disorder Symptoms

TMJ disorder symptoms can vary, affecting not only the jaw but also surrounding areas such as the face, neck, and even the ears. If you are experiencing any of the following TMJ disorder symptoms, it may indicate that your temporomandibular joint (TMJ) is not functioning properly.
Jaw Pain or Tenderness
- Aching or sharp pain localised to the jaw is a common TMJ disorder symptom, which can affect one or both sides of the face, near the ears.
- Radiating pain may occur as the discomfort spreads to the neck, shoulders, or facial muscles, resulting in a dull, constant ache.
Clicking or Popping Sounds
- Clicking, popping, or grating sounds are common TMJ disorder symptoms that often occur when the jaw joint moves, such as during chewing, talking, or yawning.
- Inconsistent noises may be accompanied by sensations of the jaw shifting or locking, further indicating TMJ disorder symptoms.
Headaches or Earaches
- Due to muscle strain and tension in the jaw area, individuals with TMJ disorder symptoms often experience tension-type headaches, particularly around the temples or forehead.
- Sharp discomfort around the ear or a sensation of fullness in the ear can accompany TMJ disorder symptoms, and this may also be accompanied by ringing in the ears (tinnitus), a common symptom linked to the condition.
Jaw Stiffness or a “Locked” Jaw
- Muscle tightness often occurs as a result of increased muscle tension in the jaw and surrounding areas, making it difficult to open or close the mouth, especially when chewing or talking.
- Restricted jaw movement, whether it’s the inability to fully open or close the mouth or a feeling of the jaw being “locked,” can make eating, speaking, or yawning uncomfortable.
Swelling Around the Jaw Area
- Swelling around the TMJ is another common TMJ disorder symptom, as the jaw joint may become swollen due to irritation or inflammation, making it painful to move the jaw.
- The area around the jaw may experience tenderness, feeling sensitive or swollen when touched, further indicating joint dysfunction.
How We Treat TMJ Dysfunction

Our therapists guide you through targeted exercises to stretch and strengthen the muscles around your jaw, reducing pain and restoring normal movement. Low-load exercises are also prescribed to improve joint mobility without putting excess pressure on the TMJ.
1. Physiotherapy
Our therapists guide you through targeted exercises to stretch and strengthen the muscles around your jaw, reducing pain and restoring normal movement. Low-load exercises are also prescribed to improve joint mobility without putting excess pressure on the TMJ.
For a comprehensive understanding of how these techniques complement broader physiotherapy practices, browse our full range of services and discover how they can benefit your overall health and mobility.
2. Manual Therapy
Manual therapy focuses on gently manipulating the jaw to restore natural movement, break up scar tissue, and relieve tension in the surrounding muscles. This hands-on approach can alleviate tightness and improve your range of motion.
3. Shockwave Therapy
We use shockwave therapy to improve TMJ joint movement and alleviate pain. By stimulating blood flow and promoting healing, this cutting-edge treatment helps reduce inflammation and speed up recovery. It is particularly beneficial for chronic TMJ conditions that don’t respond well to traditional therapies.
4. Cryotherapy and Heat Therapy
To relieve acute pain, we may recommend applying cryotherapy (cold treatment) or heat to the affected area. Both techniques help reduce inflammation, promote circulation, and provide quick relief from discomfort.
5. Intraoral Manual Therapy
For some patients, intraoral manual therapy is used to stretch the jaw from inside the mouth, helping restore normal function and flexibility to the jaw joint and surrounding muscles.
Prevention and Long-Term Care
At Orchard Health Clinic, we don’t just focus on immediate pain relief; we also aim to prevent future flare-ups. Our specialists provide guidance on:
- Posture correction to reduce strain on your jaw
- Stress management techniques to minimize clenching or grinding
- Teeth grinding solutions such as mouthguards, to protect the TMJ from further damage
Why Early Treatment Matters
Untreated TMJ dysfunction can lead to chronic pain, difficulty eating, and even damage to the joint over time. Early intervention is crucial to prevent these complications and improve your quality of life. By choosing Orchard Health Clinic, you’ll receive effective, personalized care that helps you recover quickly and safely.